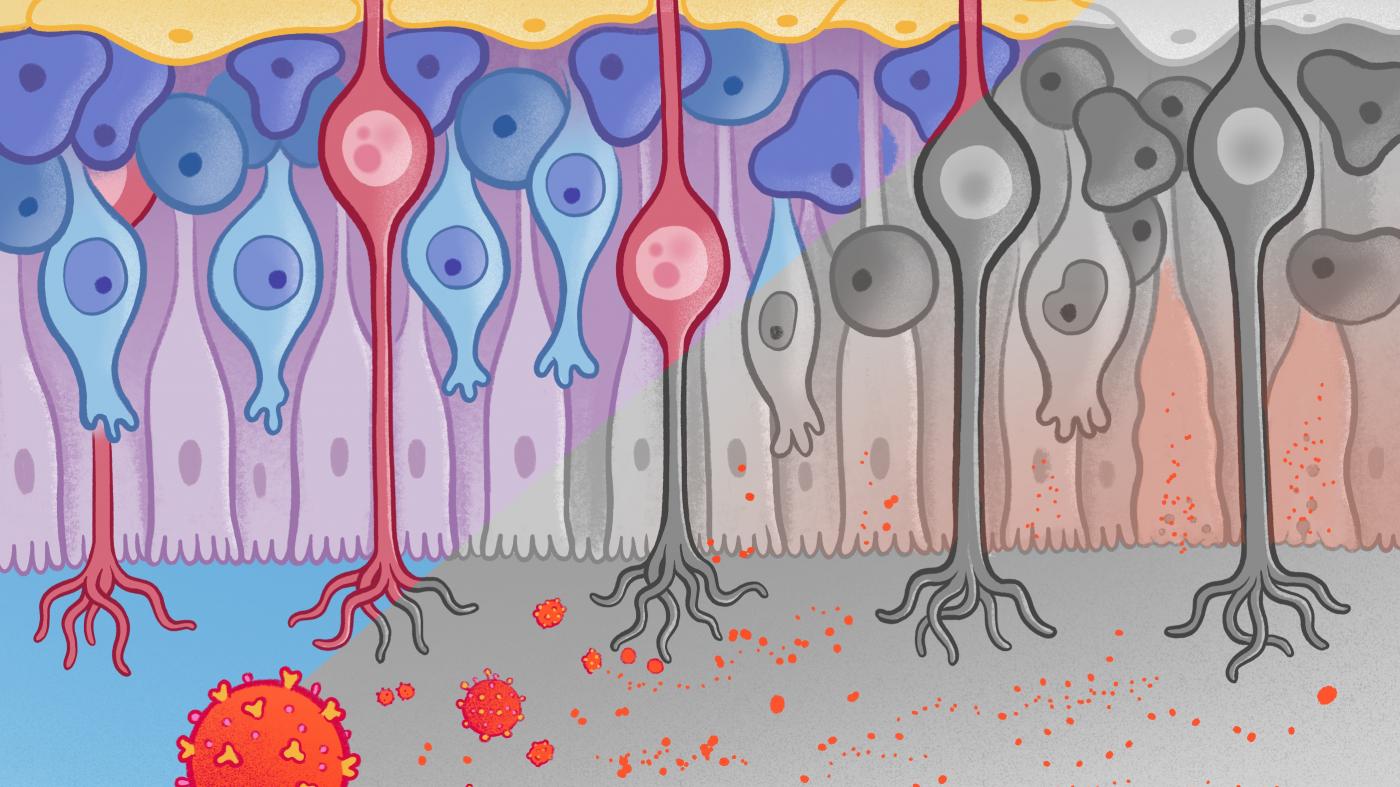
NEW YORK — The loss of smell has been a signature symptom for many people infected by SARS-CoV-2, the virus that causes COVID-19. A mug of coffee comes off as hot water. Chocolate, suddenly without its alluring aroma, loses its appeal. For most, these olfactory deficits, referred to as anosmia, last for weeks or months, but for others the losses persist. How the virus causes this symptom has been a mystery.
Now, researchers have found that the virus can rearrange chromosomes in the cells that connect the nose to the brain, olfactory sensory neurons. A collaboration of 19 scientists across Columbia University and other research institutions in New York, California and Texas reports the discovery online February 2, 2022, in the journal Cell.
The key finding centers on dramatic disruptions in the ways chromosomes self-organize and form interconnections inside olfactory neurons. In healthy neurons, these chromosomal arrangements direct the production of olfactory receptors on the cells’ surfaces. These receptors are proteins that latch onto odor molecules wafting into the nose, such as ones that give coffee, chocolate and oranges their distinctive aromas. SARS-CoV-2 infections appear to wreck the must-have chromosomal organizations.
What’s more, the apparent dependence of smell on these fragile genomic connections suggests that monitoring our smell may give us early warning of disease onset; in the researchers’ words, “olfaction may act as ‘a canary in the coalmine’ for a variety of human conditions, from viral infections to neurodegeneration."
“Not only does this work reveal the mechanism underlying anosmia caused by COVID-19, but the findings could help us uncover relationships between olfaction and diseases, including Alzheimer’s and other neurodegenerative conditions,” said Stavros Lomvardas, PhD, co-corresponding author of the paper and Herbert and Florence Irving Professor at the Zuckerman Institute.
Olfaction may act as ‘a canary in the coalmine’ for a variety of human conditions, from viral infections to neurodegeneration.
Smell Interrupted
When Marianna Zazhytska, PhD, a co-first author and postdoctoral research scientist in the Lomvardas lab, joined the hunt for the cause of COVID-induced anosmia, she happened onto a biological mystery.
“Somehow, infections with SARS-CoV-2 can cause anosmia even though we know the virus enters only a very small percentage of the olfactory sensory neurons,” Dr. Zazhytska said. “This indicates there is another way the virus is shutting down smell.”
To piece together the missing explanation, the collaboration turned to a rodent model whose cells are infiltrated by SARS-CoV-2 via portals that are especially similar to those of people. To further confirm the relevance of the animal studies to people, collaborator Jonathan Overdevest, MD, of Columbia University Irving Medical Center examined olfactory tissue from people who had died of COVID-19. The studies reinforced each other and pointed directly to how infections interrupt smell.
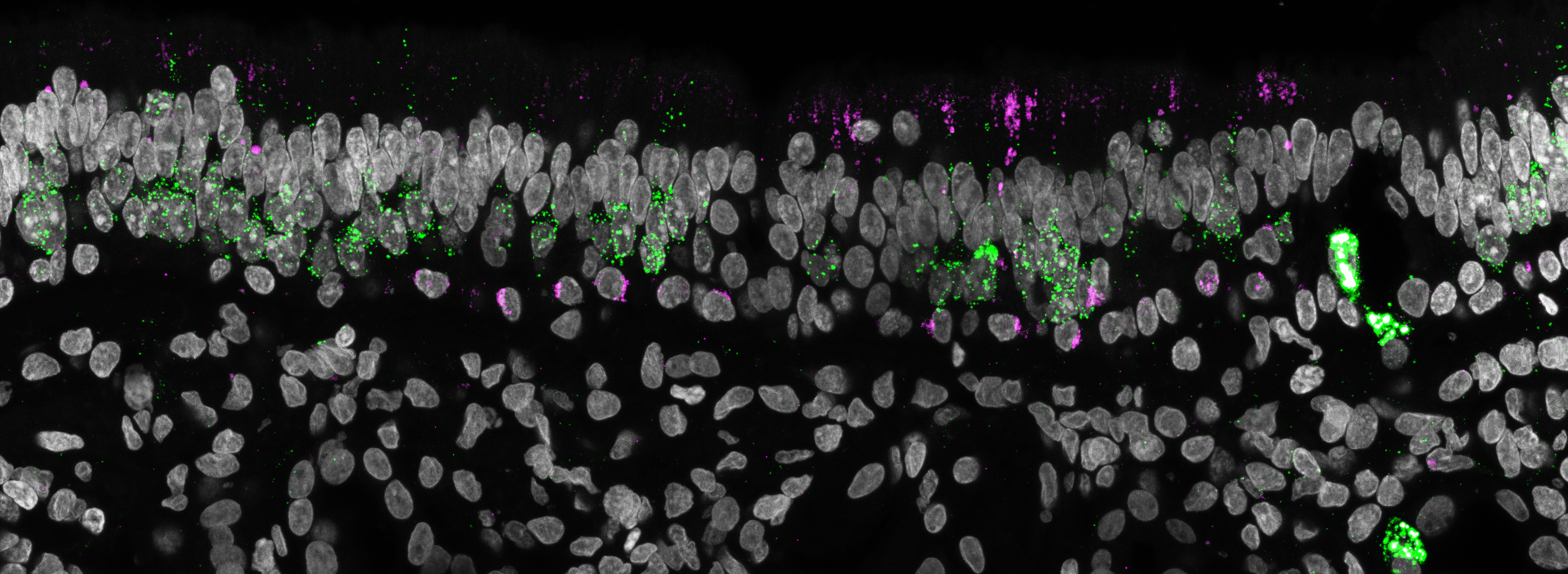
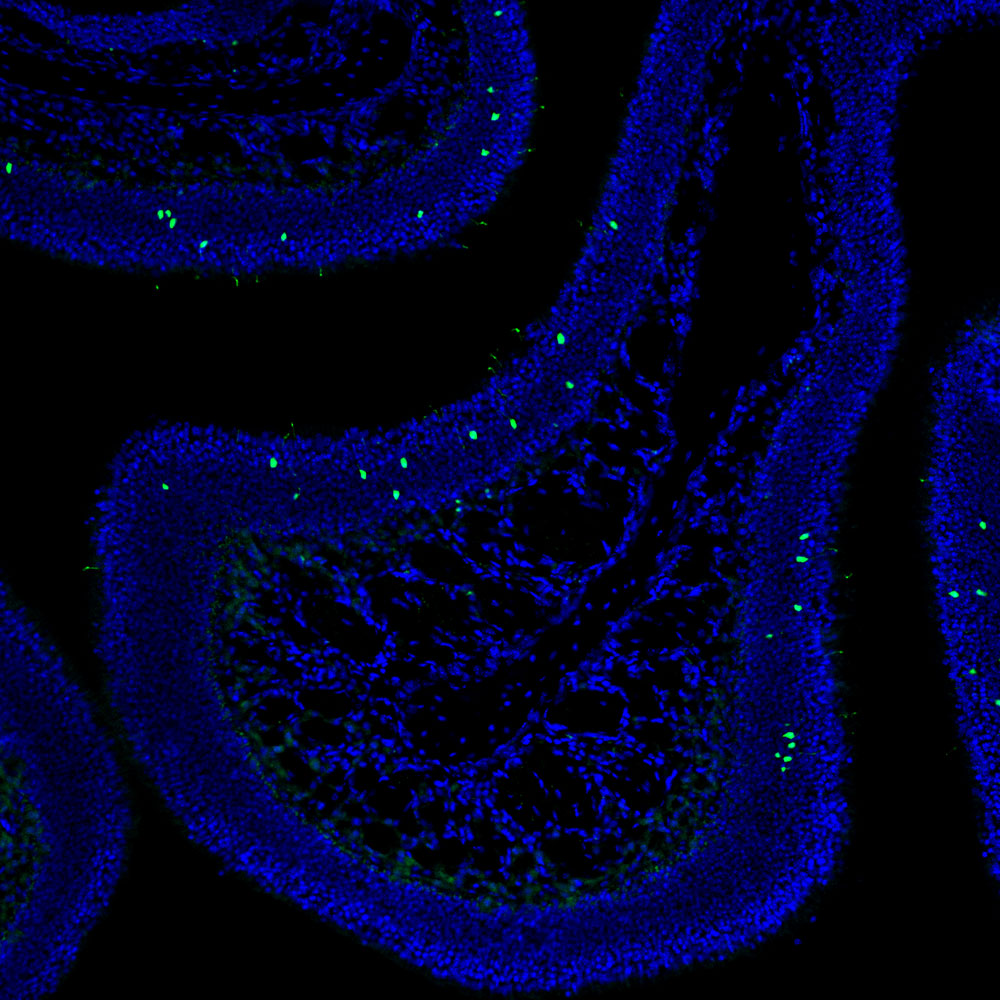
Micrograph of human olfactory epithelium from COVID-19 patient labeling SARS-CoV-2 in magenta and olfactory neurons in green. SARS-CoV-2 is detected in the apical layer and does not colocalize with olfactory neurons. (Credit: Albana Kodra | Lomvardas lab | Columbia’s Zuckerman Institute)
As the researchers now see it, SARS-CoV-2 particles enter the olfactory system not through the sensory cells, but through supporting cells known as sustentacular (SUS) cells. SUS cells form a bed of support for the nose’s sensory neurons, which normally are studded with many thousands of odor receptors. With a bevy of molecular, imaging and data-analysis tools, the researchers searched for changes inside the neurons that greatly reduce the production of odor receptors.
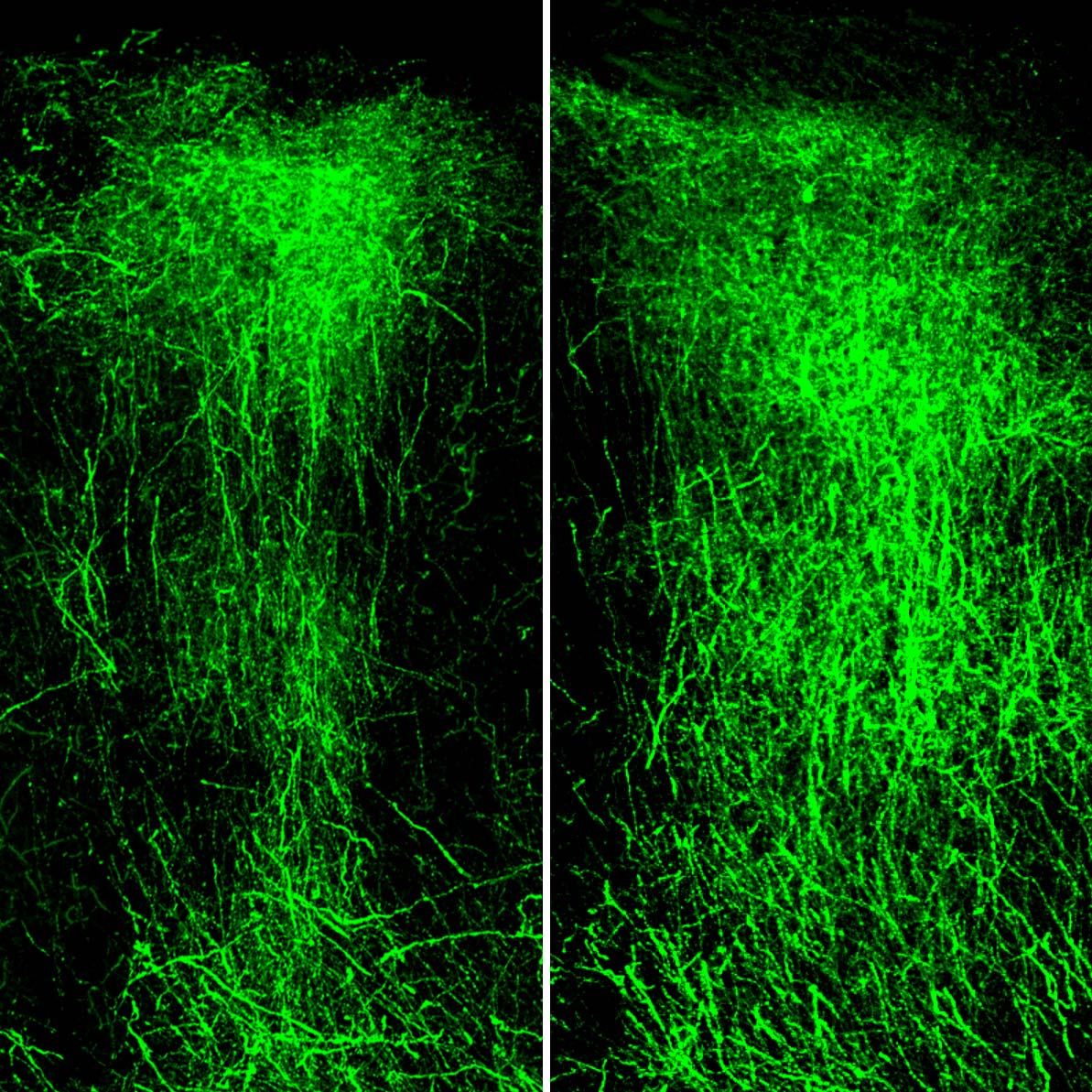
Drawing on their expertise in studying how chromosomes arrange into larger structures within the hearts of cells, their nuclei, Dr. Zazhytska and co-first author Albana Kodra found signs of trouble. Specifically, they detected cracks in the three-dimensional architectures assumed by the six-feet worth of DNA packed into the minuscule nuclei of the olfactory neurons.
“The genome contains thousands of genes for odor receptors, so we thought this damage, which reminds me of a collapsed house of cards, could impact smell,” said Kodra, a graduate student in the Lomvardas lab at Columbia’s Zuckerman Institute.
In healthy cells, the nuclear architecture includes features in which otherwise distant portions of many chromosomes are brought close together into the same space. These portions often initially reside at great distances from each other along individual chromosomes (like towns along a winding state highway) or on different chromosomes (like towns located along different state highways). Once these genetic portions are gathered this way in the nuclei of olfactory neurons, a cell’s gene-activating machinery can kick in and set the normal receptor-manufacturing process in motion.
“What surprised us in our research,” said Dr. Zazhytska, “is that the nuclear architecture gets shattered in the sensory neurons even though it’s the sustentacular cells, not the neurons, that get infected.”
As a result of this genomic damage, the researchers found, genes of olfactory receptors and other olfaction-related molecules dial way down. For people, the result of all of this infection-triggered cellular and molecular chaos is anosmia.
As always in science, new answers beget new questions. “We still don’t know what specific molecules and pathways follow the initial infection to trigger these changes in the nuclear architecture,” said Kodra.
The research, Dr. Lomvardas emphasized, was made possible by a collaboration between scientists at Columbia’s Zuckerman Institute interested in the fundamental operations of the brain and researchers at Columbia’s medical campus focused on disease. Building this bridge allowed the team to eke from the global trauma of COVID-19 an opportunity to make fundamental discoveries about olfaction that could apply to a range of diseases.
Combining the molecular analysis of human autopsies collected by Dr. Overdevest and his colleagues at CUIMC, with the animal model of COVID-19 infection developed by the group of Benjamin tenOever, PhD, at the Icahn School of Medicine at Mt. Sinai, the collaboration was able to make inroads to the understanding of neurological symptoms caused by a virus that does not infect neurons.
“We hope this new knowledge could lead to a better understanding, and maybe to diagnostic tools and treatments, for a number of conditions that involve damage to fragile nuclear architectures,” said Dr. Lomvardas, who is also a professor of biochemistry and molecular biophysics and neuroscience at Columbia's Vagelos College of Physicians and Surgeons.
###
This paper is titled “Non-cell autonomous disruption of nuclear architecture as a potential cause of COVID-19 induced anosmia.”
Additional contributors include Daisy A. Hoagland, Justin Frere, John F. Fullard, Hani Shayya, Natalie Gillian McArthur, Rasmus Moeller, Skyler Uhl, Arina D. Omer, Max E. Gottesman, Stuart Firestein, Qizhi Gong, Peter D. Canoll, James E. Goldman, and Panos Roussos.
The authors declare no competing interests.
Critical funding for this work was provided by the Zegar Family Foundation, as well as the following sources: NIDCD 3R01DC018744-01S1; U01DA052783; and HHMI Faculty Scholar Award.